 Life & Style
Life & Style

Việt Nam has made extraordinary efforts to contain the COVID-19 disease. While the epicentres have spread from China to South Korea, Iran, Italy and now the rest of Europe, with other Southeast Asian countries reporting new cases. This success of infection control has been accomplished through the mobilsation of the whole healthcare system and civil society with an ambitious programme for early detection, contact tracing and implementing early isolation and quarantine of suspected and confirmed cases.
Việt Nam has made extraordinary efforts to contain the COVID-19 disease. While the epicentres have spread from China to South Korea, Iran, Italy and now the rest of Europe, with other Southeast Asian countries reporting new cases. This success of infection control has been accomplished through the mobilisation of the whole healthcare system and civil society with an ambitious programme for early detection, contact tracing and implementing early isolation and quarantine of suspected and confirmed cases.

|
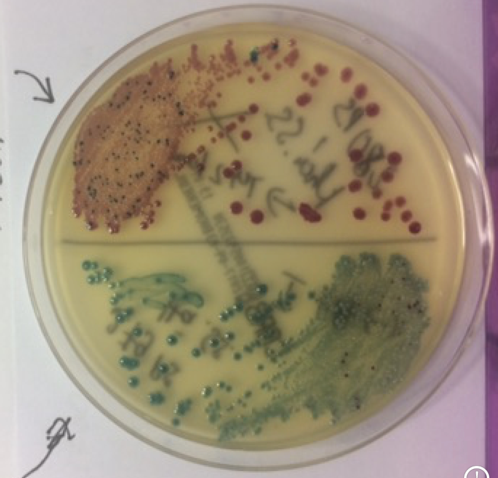
| Neonatal patients with Hospital Acquired Infection caused by carbapenem resistant Klebsiella Pneumoniae “Superbug”. — Photo courtesy of the writers |
The question then arises – what if Việt Nam could apply the same determination in other areas where we know there are preventable measures. Can the same measures be applied for the prevention of multi-antibiotic resistant “superbugs” that cause severe infections with long hospital treatment time, high mortality and costs?
In Việt Nam there is a high unnecessary use of antibiotics in the community. Many viral infections are treated with antibiotics, hence creating selective pressure for antibiotic resistant bacteria. Working as a doctor I see many patients who have been prescribed antibiotics for common cold and viral otitis. In my doctoral thesis 20 years ago, I assessed antibiotic use in a rural community outside Hà Nội, and 75 per cent of children had used antibiotics within one month, most bought from private pharmacies. We also assessed antibiotic resistance in bacteria from the respiratory and intestinal tracts and found high levels of resistance, as we repeated the study several times we could predict the increasing difficulty to treat infections – and our predictions came true. In the short term, it is cost effective to let private clinics and pharmacies with poor diagnostic capacity provide medication without a firm diagnosis – but in the long term it has consequences on the ability to treat infections – as we see now.
In 2012, we did a study in 16 hospitals throughout Việt Nam with more than 5,000 patients, and found that one third of ICU patients had Hospital Acquired Infections, most with “superbugs” resistant to the most available antibiotics. We recently also checked how many actually were colonised with “superbugs” called carbapenem resistant Enterobacteriaceae, for short CRE, in 12 hospitals, and more than 2,000 patients were colonised with CRE. At admission, 13 per cent were CRE colonised and after two weeks in care there were 89 per cent. There was a clear correlation between being colonised, getting Hospital Acquired Infections and mortality. In neonatal care about half of all patients who got infections with these bacteria die. It is estimated that 35,000 people die in Europe each year and most of Europe does not have the same level of resistance and colonisation with “superbugs” as Việt Nam.
|
| No Title |
So what if superbugs were tackled with similar determination as the COVID-19 response? There is some evidence from other countries as well as some work that has been done in Việt Nam that this might work.
Through outpatient and community care we could implement the current regulations and may be able to reduce the prevalence of 'superbugs'. These steps would include antibiotics by prescription only, following international evidence-based research and guidelines, applying simple diagnostics such as full blood counts and CRP that can differentiate between viral and bacterial infections, refraining from using antibiotics for simple cold and viral otitis, and implementing the training and empowerment of private pharmacies and clinics in diagnostics.
In hospitals the same agenda as in the Covid-19 response is needed – early detection of colonisation with superbugs and isolation to prevent transmission. This can be done through admission screening and cohort or isolation care. All patients are screened for colonisation with superbugs as they are admitted to hospital and those positive are isolated so they don’t spread the superbugs. Also improved hygiene like hand washing. This has been tested in other settings, e.g in Israel, there was a nationwide epidemic with superbugs and it was demonstrated that superbug infection could be reduced with these measures.
In Việt Nam we did an admission screening cohort care intervention at three paediatric intensive care units and demonstrated transmission reduction to almost half, which also decreased hospital acquired infections. We calculated that this saved 12 lives and about US$500,000 per 1,000 patients for the cost of approximately $3 per patient. Applied throughout the whole health system, this could save many lives and conserve resources.
Unfortunately, the intervention could not continue after the research, as the healthcare insurers could not refund the costs. Enabling hospitals and patients to be reimbursed from health insurance is highly cost effective, the hospitals can increase patient safety.
Việt Nam has now shown what can be done with a determined nationwide approach. Applying this in other urgent areas to reduce antibiotic resistance, transmission of superbugs and mortality could also be the same success story as the virus response. So – what can you as a private person do? See that you go to healthcare facilities that have the capacity to correctly diagnose and do not prescribe unnecessary medication – such as antibiotics for viral infections – that can cause adverse effects. When in hospital, check for infection control measures such as alcoholic hand rub and tend to your own hygiene. — Family Medical Practice
Authors
Mattias Larsson, MD, PhD, Associate Professor, Family Medical Practice Hanoi, Global Department of Global Public Health, Karolinska Institutet, Stockholm, Honorary Professor, Hanoi Medical University
William Brian McNaull, MD, MPhil (Cantab), DTM&H (London), Medical Director, Family Medical Practice Hanoi
For more advice on any medical topics, visit Family Medical Practice Hanoi at: 298 I Kim Mã, Ba Đình. Tel: (024) 3843 0748. E: hanoi@Việt Nammedicalpractice.com.
FMP’s downtown Hồ Chí Minh location is: Diamond Plaza, 34 Lê Duẩn, District 1; 95 Thảo Điền Street, District 2. Tel: (028) 38227848. E: hcmc@Việt Nammedicalpractice.com
FMP Đà Nẵng is located at 96-98 Nguyễn Văn Linh Street, Hải Châu District, Đà Nẵng. Tel: (0236) 3582 699. E: danang@Việt Nammedicalpractice.com









